Consortium Study of Dohner Hierarchical Classification of Chronic Lymphocytic Leukemia Reveals Improved Survival
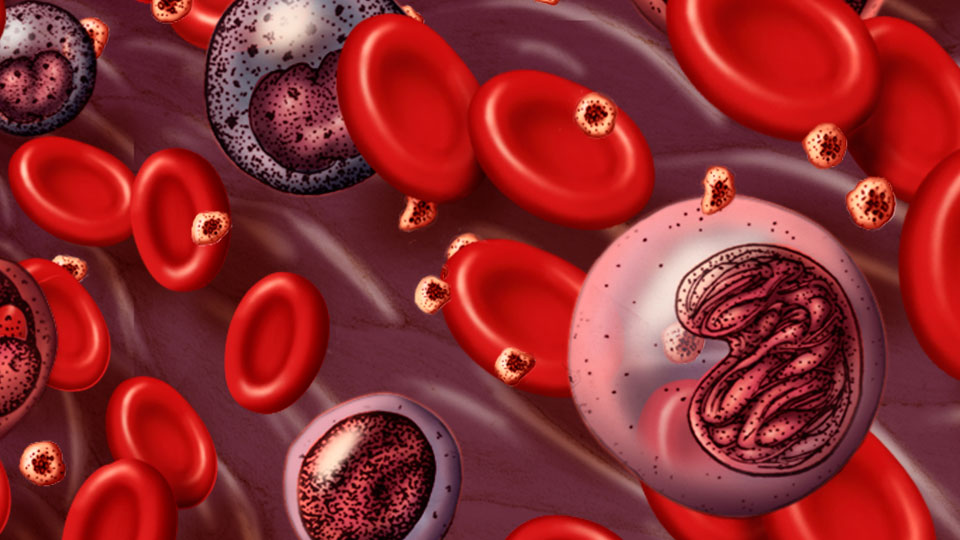
Back in 2000, a German study guided by Hartmut Dohner, M.D., established the prognostic association of chromosome abnormalities identified by fluorescence in situ hybridization (FISH) analysis in patients with chronic lymphocytic leukemia (CLL). Since then, the “Dohner hierarchical classification” has been the gold standard by which clinicians in both academic and community settings treat and counsel their CLL patients. Now, more than 15 years later, a multi-institutional study, led by Mayo Clinic, revisited the Dohner hierarchy. Why? To learn if the original prognostic association still holds true. According to the new study, this FISH hierarchy has indeed stood the test of time. Further, overall survival is now significantly longer in CLL patients—at least partly due to improved therapeutic options.
“The German study, which included 325 untreated and previously treated patients, was based on patient survival up to that time,” says Daniel Van Dyke, Ph.D., a Mayo geneticist and first author on the study paper (published in the British Journal of Haematology). “Since there have been many new therapies introduced, it was important to re-examine the prognostic hierarchy. What we learned is that therapies made available after 2000 have dramatically improved survival for all patients with CLL.”
The Mayo-led study took advantage of a robust clinical database that is part of the Chronic Lymphocytic Leukemia Research Consortium (CRC), a program project dedicated to the conduct of basic and translational research in CLL. The study included a cohort of nearly 1,600 well-documented CLL patients—more than 1,000 of whom were followed since their original diagnosis.
“Participating in a consortium offers the benefit of larger sample sizes,” says Dr. Van Dyke. “By pooling our resources, we were able to get larger numbers, and thereby ask more specific questions.”
In the new study, the relative prognostic significance of each chromosome abnormality was similar to that of the German study: The most favorable group represents patients with only a chromosome 13q deletion, and the least favorable group comprises patients with a chromosome 11q or 17p deletion. These three FISH-detectable defects retain their original 2000 hierarchy.
“There are several ways one could express the improved survival,” says Dr. Van Dyke.
“Compared to 50% of patients in Dohner’s 13q-deletion group who were still alive at 12 years, today, 80% of this group is still alive [at 12 years]. And compared to those with 17p deletion who had a median survival of 3 years in the 2000 study, our patient cohort had an improved median of 5 years.”
Whereas the median survival of all groups was 3 years in the original study, that median survival is now closer to 7 years.
One major difference between the two studies is that “we found the percentage of abnormal cells for certain FISH defects in the panel impacts prognosis,” says Dr. Van Dyke. For example, patients with 17p deletion in fewer than 20% of their cells have a favorable median time to treatment of 44 months, compared with less than 8 months for those with more than 20% abnormal cells. On the other hand, patients with 13q deletion in more than 85% of their cells have a significantly shorter time to first treatment than those with fewer than 85% abnormal cells.
Studies like these help physicians provide a measure of prognostic information for an individual patient and guide treatment. By identifying CLL patients who should, or should not, receive specific (and often expensive) therapies, this additional level of prognostication can create downstream savings for the total cost of care.
“A patient who presents with a 13q deletion might, to the clinician, look exactly like a patient with a 17p deletion,” says Dr. Van Dyke. “So you do a FISH study, and if you see the patient only has chromosome 13q deletion, you can be more optimistic and perhaps only see that patient once a year. But if the CLL cells have an 11q or 17p deletion, then more frequent follow-up is warranted, so treatment can be initiated when needed.”
Also, for patients with 17p deletion, standard therapies such as FCR (fludarabine, cyclophosphamide, and rituximab) should not be given to them, as the response is too brief; other options need to be sought for those patients.
Moving forward, Dr. Van Dyke is optimistic. “New drugs have been introduced since many of our CRC study patients were originally treated, and they’re going to be even more beneficial,” he says. “For example, the novel signal inhibitors such as ibrutinib, acalabrutinib (ACP-196) and idelalisib are found in recent clinical trials to be effective even in the FISH-high-risk CLL patients.”
Client
Mayo Clinic - Mayo Medical Laboratories
Date
25 April 2016